Hamstrings tendon Injury
What is Hamstring muscle and its function?
Hamstrings are the big bulky muscle group at the back of the thigh that crosses and controls both the hip and knee. Functionally the Semimembranosus, Semitendinosus and Biceps Femoris are the three main parts of the hamstrings (Fig. 1). They originate from the Ischial tuberosity (the part of the pelvis one sits on and can feel along the buttock fold) and attach to the shin bones just below the knee joint and can be felt as strings on either side of the back of the knee. Anatomically the Adductor magnus (a muscle in the lower inner thigh) also forms part of Hamstrings originating close to the other Hamstring muscles but it does not cross the knee joint and so functionally is not similar to the three main muscles mentioned above. The Hamstrings group of muscles extends the hip as in extending the leg straight back and flexes the knee.

Fig 1
What is the mechanism of Injury?
Injury happens as the muscle is stretched beyond its capacity with a sudden load, especially when the muscle is contracting while being stretched by the sudden load. It is called eccentric contraction and typically happens during sports activities or falls resulting in near splits. It can occur in any age group but seems to be more common in adolescents and patients in their 40s and 50s.
What are the predisposing factors?
Tight hamstrings, inadequate preconditioning, inadequate warm up, fatigue from too much stress, muscle imbalance, previous hamstrings injury and certain activities like football, running and dancing are risk factors that predispose the body to Hamstrings injury.
What are the types of injury?
The type of injury is defined by the severity of injury, and it varies. Grade 1 is where a few fibres of the muscles are injured. Grade 2 is where partial muscle is injured. Grade 3 is when a complete muscle is injured. Severe Grade 3 (some surgeons call it Grade 4) is one or all three main muscles are pulled off their attachment to the ischial tuberosity and retracted.
What are the symptoms and signs?
Pain around the posterior thigh is the main symptom. Swelling and bruising will be seen depending on the extent of tendon injury. Weakness of Hamstrings will be seen and is due to pain inhibition and muscle weakness from the injury. Weightbearing can be uncomfortable in the first few days to weeks of injury occurrence. Patients presenting late will have discomfort in the ischial tuberosity region, especially while sitting. In the complete Grade 4 injury there will be weakness on stairs, push off, running and exercises that involve Hamstrings muscle.
What investigations are needed?
MRI is diagnostic of the Hamstrings injury and its severity (Fig. 2). It also shows the extent of retraction in the complete avulsion injury (muscle pulled off from its attachment) and the muscles involved. Ultrasound is operator dependant and might not give the full picture. An x-ray or CT scan might be necessary if bony avulsion (muscle pulled off with a chunk of bone from its attachment) from ischial tuberosity is suspected.
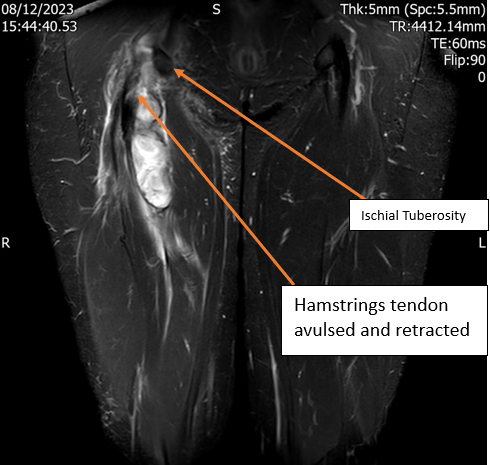
Fig 2
What are the treatment options?
In mild injuries (Grade 1 and 2) pain will settle down with rest, cold compression, analgesics and support to mobilise, if needed, in the first few days. Gentle strengthening exercises can be started, and Hamstrings strength will fully recover within 6 to 12 weeks. It is important to continue with a year-round regular exercise programme to prevent further injury.
Patients, especially young and active patients, who have complete avulsion of all muscles are likely to need surgical repair. It is ideal to have the repair done as soon as possible, but preferably within 6 weeks. If it is delayed any longer the need increases for extensive soft tissue dissection to mobilise the tendon and achieve satisfactory repair.
Patients with low demand might decide to continue with non-operative treatment, accepting certain limitations in activities due to Hamstring weakness like weakness noticed on stairs – especially when climbing.
What is involved in surgical treatment?
The aim of surgery is to:
- restore muscle strength and function
- provide pain relief
- be able to return to day to day and fitness activities as before.
The repair of Hamstrings can be performed under general or spinal anaesthesia. Patients will be lying on their front and an incision is made along the gluteal (buttock) fold. The sciatic nerve is close to the tendon but will be protected. The tendon origin point (Ischial tuberosity) and the tendon ends will be freshened. 3 or 4 suture anchors will be placed in the ischial tuberosity. The sutures will be passed through the tendons and will be tied securely approximating the tendon ends to their origin point in the ischial tuberosity. The wound will then be closed after stopping any bleeding.
What does post-operative care involve?
The Hamstrings repair will have to be protected with a hip or knee brace for 6 weeks to control tension on the tendon repair. Physiotherapists will help patients to practice with the brace prior to surgery to make it easier to mobilise with the brace after surgery. There will be restrictions on hip flexion; patients will be allowed to do gentle knee flexion exercises only. Hip extension exercises can be started after 2 weeks. Weight bearing will be between partial to full weight bearing with crutches for 6 weeks. DVT prophylaxis will be given for 2 to 6 weeks depending on the weight bearing status. Usually, patients will be discharged the next day.
Physiotherapists will take patients through a phased rehabilitation programme. At 6 weeks the brace will be removed. Hip flexion will be allowed as long as no tension is felt at the Hamstrings repair site. Active strengthening exercises for Hamstrings will then commence. Hamstrings stretches will start at 3 months. Fitness exercises will be gradually introduced between 8 to 12 weeks. Sports can resume after 3 months depending on the intensity level. Most patients will be able to return to fitness and sports activities between 3 to 6 months. It is important to maintain strength and flexibility to prevent further Hamstrings injury.
Return to work depends on the nature of work and can be anywhere between 2 to 12 weeks.
While using the brace it is not be possible to drive. Patients will be able to drive as soon as they feel able to apply sudden break. Usually this takes between 6 to 8 weeks.

Fig 3 MRI pelvis done one year after repair
What are the possible complications?
There are rare but possible complications are listed as follows:
- Deep vein thrombosis and pulmonary embolism
- Infection
- Sciatic nerve injury
- Re-rupture or weak muscles due to inadequate healing, resulting in poor function. This is more common in delayed repairs.
- Discomfort, especially while sitting
- General complications
